Emily Boerger | May 20, 2020
Health Management Associates (HMA) on Tuesday released an update to their analysis of COVID-19’s impact on health insurance coverage. The update builds off an April report that evaluated the impact of potential US unemployment rates on Medicaid, state marketplaces, employer-sponsored coverage, and the uninsured.
The updated analysis uses three different unemployment rate scenarios to estimate impacts: a “moderate” unemployment rate of 20%, a “heavy” rate of 24%, and a “severe” rate of 28%. The national pre-COVID unemployment rate was 3.5%.
HMA projects Medicaid enrollment across the nation could increase by 5 to 18 million by the end of the year, depending on changes in the economy. Projected further out, enrollment in 2022 could increase 0.5 – 4.5 million compared to enrollment numbers at the end of 2019. HMA also predicts the growth in Medicaid enrollment will cost at least $11 billion in 2020, and total state and federal costs could range from $18 billion to $127 billion between 2020 and 2022.
“While the [Families First Coronavirus Response Act]-provided 6.2 percentage point enhanced FMAP will cover much of the costs related to higher Medicaid enrollment, projected state revenue shortfalls remain a major pressure on state finances,” reads the analysis.
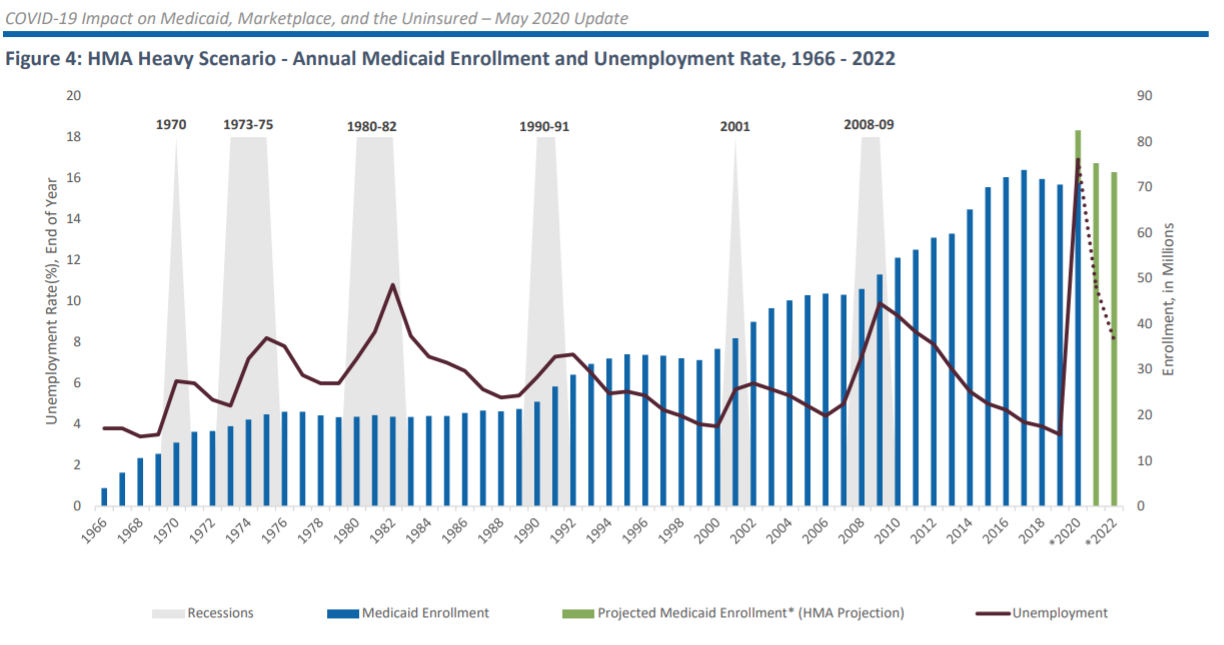
Image: Health Management Associates
The study predicts non-expansion states will see a disproportionate share of newly uninsured. These states represent 30% of individuals losing employee sponsored insurance, but HMA estimates they will make up almost 70% of the newly uninsured by the end of 2020.
The report also breaks down the increases in cost for new Medicaid enrollment by state under the three different economic scenarios.
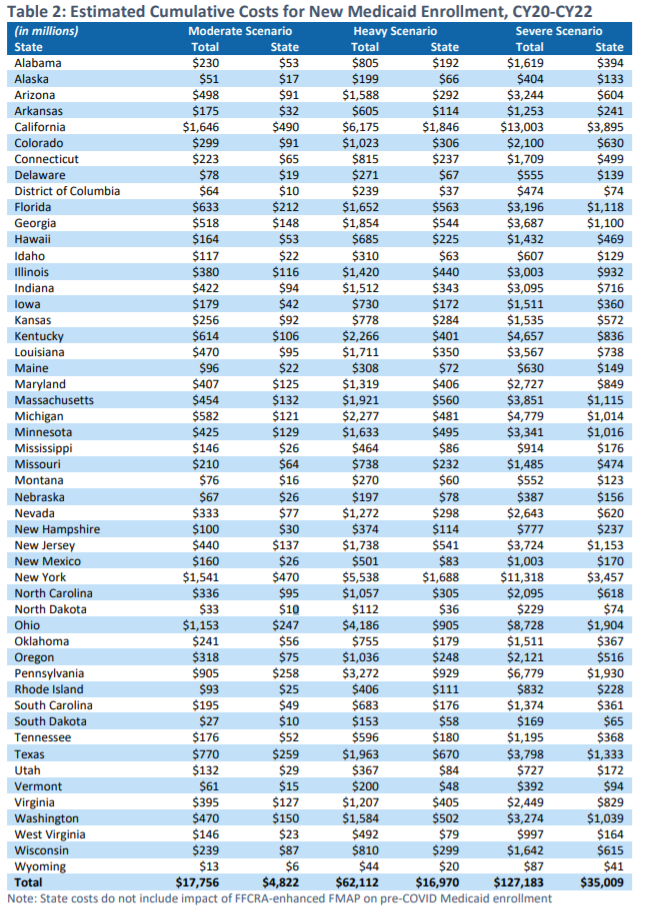
Image: Health Management Associates
HMA’s full report is available here.

