![]()
By Andy Miller
Aretha Frison got an unusually helpful mailing recently through the Louisiana food stamp program.
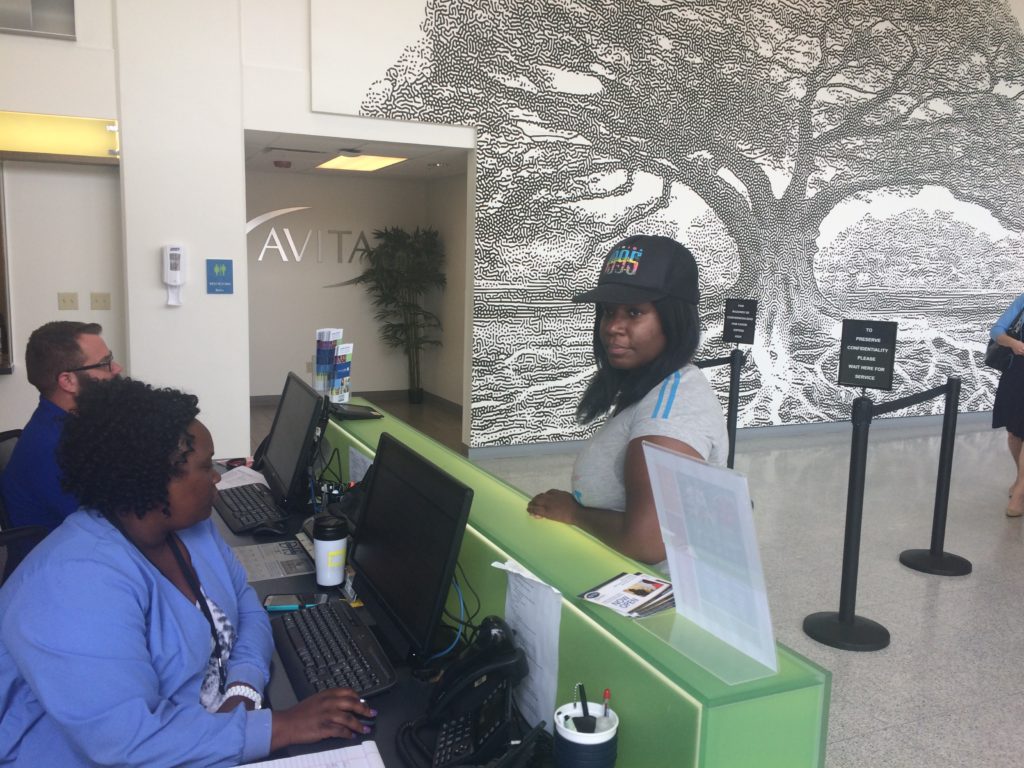
The letter indicated that she could qualify for Medicaid coverage beginning next month. Frison, usually a journalist by occupation, has been able to work only part time at an animal hospital while suffering with major depression. Rent and other expenses have been a struggle, she told reporters last week when she visited a New Orleans health clinic. She said she “has been hitting a lot of brick walls’’ when it comes to obtaining psychiatric treatment.
Aretha Frison (right) at Crescent Care. Photo credit: Andy Miller
“It’s been a tough road for me to get services,’’ said Frison, 38.
Now, though, “it seems like Medicaid is the golden ticket,’’ she said.
Frison is one of the more than 200,000 Louisianans who have signed up or been enrolled this month in the state’s newly enacted expansion of Medicaid, under the Affordable Care Act.
On July 1, Louisiana will become the 31st state to go forward with expanding the government program, which is jointly financed by state and federal governments. On his second day in office, Gov. John Bel Edwards, a Democrat who expressed support for expanding Medicaid during his campaign last year, signed an executive order that began the expansion process.
It will extend coverage to people up to 138 percent of the federal poverty level, which is $16,394 for an individual. With the move, Louisiana follows Arkansas and Kentucky as the only Southern states to adopt expansion.
Louisiana officials project that the influx of newly insured from Medicaid expansion eventually will reach 375,000. Just last Monday, 3,000 people enrolled for coverage, state officials say.
Edwards told health care reporters gathered in Baton Rouge last week that 70 percent of the people who will get coverage are full-time workers, in such industries as construction and hospitality.
“I always said Medicaid expansion is the right thing to do,’’ he said.
One argument Gov. Edwards emphasized is that prior to this year, Louisianans helped pay for Medicaid expansion in other states (through their federal taxes), but got nothing in return.
He knows the process won’t be easy. “We have the benefit of the experience of other states,” he said, but acknowledged, “I know we’re going to have some hiccups.”
A tale of two (Southern) states
Louisiana and North Carolina have many political similarities. Both states also have somewhat similar health issues affecting their populations.
And until recently, both states had similar approaches to Medicaid expansion.
Gov. Pat McCrory, a Republican, has rejected expansion since early 2013. Bobby Jindal, a Republican who was governor of Louisiana until early this year, took the same position through his eight years as chief executive.
Gov. John Bel Edwards addressed reporters earlier this month. Photo credit: Andy Miller
Under Jindal, efforts to enact expansion in Louisiana went nowhere. “For years, we were not allowed to speak [about] it,” said Jen Steele, Louisiana’s Medicaid director.
In North Carolina, anti-expansion sentiment goes beyond McCrory. In 2013, the Republican-led General Assembly added its own barrier to expansion. It passed a law that requires legislative approval — not simply a governor’s decision — for any such move in the future.
McCrory, along with legislative leaders like Senate President Pro Tempore Phil Berger (R-Eden), has repeatedly pointed to the cost of expansion, saying it eventually would put too much strain on the state budget.
Attempts by Democrats in the legislature to expand Medicaid have run into a brick wall of opposition. Of the at least four bills introduced during the 2015-16 biennium, none made it into committee meetings.
But in remarks about the recent waiver application sent to the federal Centers for Medicare and Medicaid Services, Health and Human Services Secretary Rick Brajer noted that the administration’s priority would be having North Carolina expand the program as it implements Medicaid managed care.
Brajer also noted that at every one of the dozen hearings around the state to get public feedback on the Medicaid plan, speakers asked for expansion.
And privately, some Republican legislators acknowledge some form of expansion may be needed in order to get federal approval of the Medicaid plan.
Effects on hospitals may vary
One key difference between North Carolina and Louisiana is a much stronger fiscal situation in the Tar Heel State. Louisiana, where the energy industry is very important, has been hit hard by a decline in oil prices. Edwards inherited what he calls a record state deficit.
But ironically, that deficit eased the road for expansion, officials say. “The budget crisis was a catalyst for the Legislature to come aboard,” said Dr. Rebekah Gee, secretary of the Louisiana Department of Health.
Dr. Rebekah Gee
A study found that the expansion would produce net savings of $184 million for Louisiana, including in-state money paid to hospitals, and moving some current Medicaid patients into a better federal matching rate of 95 percent.
Other states have done studies showing projected savings from expansion.
Like North Carolina, Louisiana has a population with many health needs.
America’s Health Rankings puts Louisiana 50th among states — 19 spots behind North Carolina. The state has high rates of obesity, hypertension and diabetes, and a high mortality rate from cancer.
Louisiana also has a very high share of people living in poverty, but North Carolina has 15.6 percent of citizens uninsured, compared to Louisiana’s 11.7 percent.
“This isn’t just about expanding health care coverage and saving money,’’ Edwards said. “We want healthier people in Louisiana.”
Part of the push to enroll new people in Medicaid has come through a unique mailing to 105,000 food stamp recipients, like Frison. The mailing gives them four questions to answer to determine whether they’re eligible.
About 180,000 other people were ‘’auto-enrolled’’ from a previous “waiver’’ program that did not provide coverage for hospital services or prescription drugs.
No extra state money was appropriated for marketing and publicizing Medicaid expansion, so the state cobbled together funding from the Robert Wood Johnson Foundation and other sources.
Ruth Kennedy, director of the Medicaid expansion effort, said the state also learned from the messy rollout of the ACA’s insurance exchanges in late 2013 and early 2014, when constant technical problems snarled the initial enrollment process.
“We put in a great deal of effort getting to Day Two without an absolute meltdown,” she said.
Enrollment events have brought in people like Jaylin Davis of Baton Rouge, who lost Medicaid when he turned 19. Jaylin, who works at a local Wal-Mart, told a reporter after signing up at Baton Rouge Community College that he was glad to have the chance to get the insurance coverage back.
Health plans say they are hiring dozens of new employees to handle the new enrollees. Though hospitals in other states have reported substantial revenue gains as a result of expansion, Louisiana’s complicated system of funding for hospitals may not yield many clear winners.
Louisiana has had an unusually heavy reliance on ‘’disproportionate share’’ dollars, which the state pays out to those hospitals serving a large number of indigent or uninsured patients.
While the giant Ochsner Health System said expansion would be slightly positive financially, Baton Rouge-based Our Lady of the Lake said expansion may bring a payment cut.
But low-income patients should benefit greatly.
For those who come to CrescentCare, including many with HIV, the new coverage will make significant improvements in care, staff at the New Orleans health center told reporters.
New Orleans’ Charity Hospital closed after being flooded during Hurricane Katrina and has never reopened, as Louisiana foundered financially after the storm. Photo credit: Rose Hoban
More than half of its 4,000 medical care patients may qualify for Medicaid under expansion.
Alicia Honomichl, an RN, says CrescentCare nurses currently “spend so much time coordinating services for patients.’’
She said expansion will help more people obtain PrEP, a medication that can prevent a person from getting HIV from an infected individual, whether through sexual contact or sharing of drug-injection equipment.
Dr. Peter DeBlieux, chief medical officer of the brand-new University Medical Center New Orleans, says the Medicaid change is “earth-shattering’’ for his patients.
Historically, uninsured patients went to emergency rooms for routine care — a wasteful, inefficient use of health care resources — because they had nowhere else to go, said Dr. Jennifer Avegno.
DeBlieux, who was a physician at Charity Hospital in New Orleans when it was evacuated during Hurricane Katrina in 2005, adds that patient access to regular medications will be “low-hanging fruit’’ that will come from expansion. “I expect [cancer] screenings to skyrocket.”
State officials are voicing optimism about Louisiana’s move. “I believe our approach will be a national model,” Gee said, adding that other Southern states “are watching us.”
Most Republicans at the national level remain vocal critics of expansion, and they support repeal or weakening of the ACA itself. But Edwards told reporters that if Democrats retain the White House and the health law stays in place, “I fully expect there will be a number of states opting into Medicaid expansion.”
Rose Hoban provided additional reporting on this story.
Tagged ACA, Affordable Care Act, America’s Health Rankings, cancer screening, Centers for Medicare and Medicaid Services, Gov. Pat McCrory, Medicaid expansion, Medicaid reform, Medicaid waiver, PPACA, Sec. Rick Brajer, Sen. Phil Berger